Did Biden Cause the Rise in Inflation in 2022? And Was Inflation the Real Problem?
President Biden came into office in January 2021. Inflation started to rise two months later and continued to rise to exceedingly high levels in 2022. Trump, who was planning to run for re-election in 2024, immediately blamed Biden for the inflation. Did Biden do something in the first two months of his administration to cause inflation? Is that even possible? What caused the dramatic rise in inflation? And was inflation the real problem that people confronted—or was it the cost of living, meaning that people’s income didn’t rise to meet the inflation?
Let’s be clear, there is almost nothing any President can do to cause inflation, or to stop inflation after only two months in office. Policy changes take many months, sometimes years, to affect the largest economy in the world.
“Almost” nothing? Well, there are exceptions. Policy changes are on thing, but drastic actions can be devastating. After all, you could take the best, most expensive, and modern car that takes years of planning and development—and destroy it in seconds. Just drive it over a cliff and watch. It’s the same with a society. Unconventional actions that destroy segments of normal society that took years, decades, and even centuries to build could cause unforeseen consequences that are unpredictable. But Biden took no drastic or unconventional actions in his first two months in office. He moved slowly and deliberately as his administration developed over his first six months, and then his first year. Trump blamed Biden for the inflation, but he never said what Biden did to cause it. He just repeated the accusation over and over—and people believed him.
Political observers like to say that when things go bad during a President’s term in office, it’s the President’s fault, but they only say that if their current party is out of power. And, of course, when their party is in power, they blame the previous President.
So, what did cause the inflation? Or—was inflation the real problem that caused so many people to complain about it?
The Real Problem with High Inflation is When Wages Don’t Rise to Meet It
Inflation’s real problem is about the cost of living and how wealthy you are. Inflation is no problem if your income goes up to balance it out. And the wealthier you are, the less it matters.
Take millionaires, multimillionaires, and billionaires. When the price of groceries increases, their lifestyles are not affected. Everyone in the top 10% of wealth distribution—who control 70% of America’s wealth—do not feel any changes in their lifestyle when the price of groceries goes up, for example.
On the other hand, if you are at the bottom of the income scale, or even at the middle-income level, groceries can be a major part of your necessary expenses. The more money you have, the less important groceries are to your budget.
It’s the cost of living that really matters. If there is inflation and wages go up to compensate for it, the higher prices are not felt in the middle and lower classes—and people accept it.
Every 15-20 years, prices go up 30 to 40 percent in a healthy, thriving economy and people accept that as normal. But inflation usually happens a little each year—and people don’t feel it very much. But when prices and wages stagnate for most of that period and then suddenly prices go up in a year or two, people feel the pain, and the bottom and middle classes feel it the most.
But—what is a “healthy, thriving economy”?

Can Inflation Be Good?
Economists believe that some inflation around a 2% annual average is healthy as it means the economy is growing. If it goes up one month to 2.5%—or even 3%—economists don’t think that’s bad, but they start to examine the causes to see if it’s an anomaly—or the beginning of a trend. And if it suddenly goes down one month, it could lead to deflation (when inflation is below zero). They keep an eye on that for the same reasons: Is it a trend or an exception? *
Some people say that inflation is caused by national debt, which is now at record levels. As a general statement, they are wrong. That can happen, but if that were true in all cases, then every time the debt went up, inflation would follow. But history proves that’s not always the case. One example alone disproves this theory. After WWII, when the national debt in the U.S. was the highest it has ever been when measured against the country’s total wealth (including our present era), the economy boomed for the next three decades. Not only that, after the war, with GIs returning to the workforce, demand for everything was extremely high. And high demand can be a major factor in inflation. But there was no major inflation right after the war or in the following decades. The 1960s was the largest boom in American history. And taxes after the war, and up through the 60s, were at the highest level in history, especially for the wealthy. These high taxes also brought on balanced budgets.
Another more recent example is what happened since the Iraq/Afghanistan wars. Military spending went up starting with the invasion of Afghanistan in 2002, followed by the invasion of Iraq in 2003. War costs went into the billions. Taxes were lowered just prior to the war, and the national debt skyrocketed, yet there was no high inflation from the start of the wars up until 2021, although the national debt from 2003 up until 2000 went up dramatically by trillions.
National debt can definitely contribute to inflation, but to say it is the cause of inflation is naïve, even ignorant—or maybe some people just want to believe that that is the cause, so they push that statement.

Major debt like we have now is not good, but it’s not just a spending issue. It’s an income issue as well. And almost all income comes from taxes. President Eisenhauer, when he was in office in the 1950s, always resisted lowering taxes, saying the national debt would go up. In 1960, income over $200,000 was taxed at 91%. (That $200,000 would be worth $2 million in today’s dollars, meaning income over that amount would be taxed at 91%.)
What can happen quickly is economic crashes. They can happen almost immediately. It’s like a car. It takes a lot of planning and work to design and build a great car, but it can all be destroyed in an accident in seconds. But car accidents also have causes. A crash is what happened over a noticeably short period of time in 2008 when the “Great Recession” came about. But its causes go back many years.
How Much Do Prices Naturally Increase Over Time in a Healthy Economy?
Another crucial factor in dealing with inflation is how much inflation rises over time in a healthy economy. With a healthy 2% inflation rate per year, that means that over a 14-year period, inflation would cause prices to rise at least 28% (2% times 14), but the inflation rate would be compounding. Consequently, there would be approximately a 30% increase in prices. Let’s take a look at how prices changed from the Great Recession prices in 2008 up through the high-inflation year of 2022, a 14-year period.
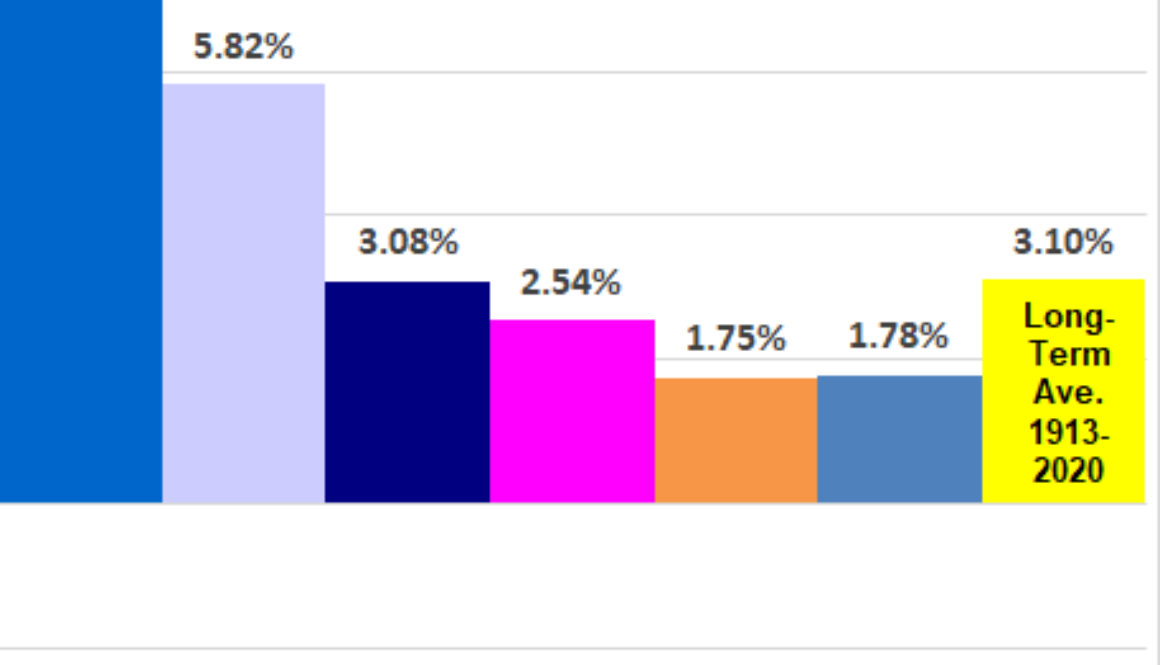
In late 2008, the “Great Recession” started. That year, inflation started to drop drastically in November and December and continued to stay low for the next 10 years until it climbed slowly upward until 2022—14-years later—when it had a dramatic rise. The average annual inflation rate during those 14 years was very low at 2.25%. In 2022, the last year of that 14-year period, the average inflation was 8%. That’s quite an increase in one year when you consider that annual healthy inflation should be around 2%. But overall, an average of 2.25% per year is very low. Even if it had been 3% average per year, that would not be alarming.
“Average inflation 2008-2022 was low, but it all hit in one year”
Another way to look at it is that prices at the end of 2022 were pretty much where they would have been if there had been no Great Recession and no Pandemic—and the economy was healthy and growing during that period—with inflation occurring at a normal, healthy annual rate—instead of happening all in one year, which is what happened in 2022. In other words, inflation was not a big deal when you look at the long-term average. In fact, that 14-year rate was one of the lowest inflation rates experienced over a similar amount of time in the previous 50 years.
“The real problem with inflation is when wages don’t go up”
But in 2022, people complained about the inflation in the cost of basics, especially for necessary products like food. But if the average rate was normal over 14 years, why would people complain? For a very simple reason: It was because the cost of living went up drastically. Wages and employment were stagnant and very low during that 14-year period. Many lost their jobs and couldn’t find work. It was labeled the “Great Recession” for a reason. Consequently, the pain for the average wage earner when inflation went up was quite high—and it happened all at once. In other words, inflation was not the problem. It was that the cost of living went up considerably and wages did not rise to meet the rise in prices.
Whose Policies Caused High Inflation in 2022?
Trump blamed Biden, but it’s more than likely that the inflation was caused over a period of several years before Biden became President. Trump was President for the four years before Biden. After all, there is no policy that any President could implement to cause inflation after only two months in office—even if they tried to make that happen.
If Biden caused it, Trump never gave reasons why he believed Biden caused the inflation in two months. He just blamed Biden and kept blaming him for the next four years. Trump was like a broken record. After a while, people believe it. But blaming someone is meaningless without naming the cause, although it got Trump re-elected in 2024 because he repeated the accusation over and over for four years—and Biden and the Democrats never fought back.
“People just believed that since the inflation happened when Biden was President, it must be his fault”
Just because people believed Trump’s accusations doesn’t mean he was right. We will learn below that he was wrong. Besides, as mentioned above, inflation wasn’t the big problem; It was the increased cost of living for most Americans—and of course that always affects the middle and lower classes the most.
And if Trump caused the inflation just two months after he left office, then what did he do during his four years that could have caused it?
Trump had other reasons for blaming Biden. He was running for re-election in 2024. Of course he wanted to blame Biden, who beat him in 2020.
The Seeds of Inflation Were Planted Years Earlier
In reality, the seeds of the high inflation in 2021-22 were planted years before—in 2008. That was the year that the “Great Recession” was “born” (although it was developing in the American economic “womb” for many years prior to that).
When Obama took office in January 2009, he inherited an economy in deep trouble. It was named the “Great Recession” because it was the biggest economic downturn since the Great Depression in the 1930s. Over the next eight years, under the Obama administration, the economy slowly, but surely, grew and came back. It’s like putting the car back together after an accident destroyed it. It’s a slow process—and you can’t just go out and buy a new economy.
By the time Trump took office in 2017, all economic indicators showed a healthy economy solidly on the road of recovery; Employment was coming back, along with the stock market. Inflation was exceptionally low during the previous nine years, even dipping into negative inflation, i.e., deflation, in 2009 and again in 2015.
As the economy improved, interest rates were raised—before Trump took office. The economy was doing well enough that Federal Reserve Chairwoman Yellen raised the rate in 2015 for the first time since 2008—in anticipation of a probable rise in inflation if they weren’t raised. The economy was doing that well.
Raising the interest rate in a recovery is done for only one reason: to stave off inflation during an economic recovery. It is done gradually so that there is no massive and sudden decrease in spending because the cost of money increased—which could cause the country to slip back into a recession. Yellen also indicated that she would continue to raise the rate in the coming years, and it was raised regularly over the next three years, reaching 2.4% by early 2019. But in 2018, President Trump appointed a new chairperson, Jerome Powell.
A New Fed Chairperson Comes to Office in 2018
Powell first indicated he would continue to raise the rates that Yellen started. But Trump did not want to. In fact, Trump wanted them lowered and—against the advice of many economists—he urged Powell to lower the interest rate, which he did three times—something that is never done when an economy is growing because of the probability of increasing inflation. Interest rates are the main tool that economists use to control inflation. But Trump had an election coming up and was afraid of an economic downturn in the fourth year of his Presidency if interest rates went up, or even just stayed where they were.
The President does not control the Fed rate. The Fed chairperson leads a board of governors who make the final decision, but the chairperson has the most power, and his term lasts four years, but it does not coincide with the President’s four years in office. It is intended to be independent so that the rate is non-political. But President Trump put pressure on Powell to lower the rates. Consequently, due to his urging, Powell lowered the rates in 2019† and were down to 1.5% by early 2020 (when the Pandemic started). The Fed looks at long-term trends. Trump was looking at the short-term effect on his re-election.
When Trump took office, he claimed he inherited an economy in 2017 that was a “mess.” But in reality, all indicators showed a strong stock market, growing employment and steady economic improvement when he took office. Trump knew it, but he wanted to take the credit for its revival since it was already happening. It was classic “Trump speak.” Consequently, he called it a “mess” shortly after his inauguration in 2017. After all, he was already thinking about his re-election.
But he was wrong. The “mess” was in 2008. The economy in 2016 was solidly on the road of recovery and was doing well.
Trump Economic Policy 2017-2019
In the first three years during Trump’s administration, the economy continued to improve with low inflation—all because of a decade of sound economic policies instituted before Trump.
Trump only made two major economic policy changes during those first three years (his fourth year was the pandemic year). First, in 2017, he lowered taxes for the wealthy, which increased the national debt substantially over the coming years. Trump claimed that he lowered the taxes for the middle and lower classes, but it was so small that it was Trump’s gesture to them, because most of the tax reduction went to the wealthy, which included Trump himself, along with his family.
But a big problem was that unemployment, which had gone down in recent years, was still above ideal and wages for the middle and lower classes were stagnant in most of the years since the Great Recession. And who cares about reducing your income taxes when you are unemployed?

Regardless, the tax reduction for the rich was another input into the economy of cash that would add fuel to the fire of inflation right after Trump left office in January 2020. Tax deductions are always an input of cash, delivered and processed in the hands of the wealthy. And they always take time to make their way into the economy because taxes are always paid a year or more in the future after they become law.
Interest Rates Under President Trump
Trump’s second major economic change was to persuade Powell— against the advice of almost all economists— to lower the interest rates after they were recently raised. Lowering interest rates is an economic tool that is used to help jump-start when the economy goes into a recession. The country at that point was coming out of a recession and in such good shape that interest rates had been lowered before Trump became President. The economy was already improving and far along the road of recovery from the Great Recession. Raising rates during a recovery is done to stop possible inflation. Trump did the opposite—because he was afraid of not getting re-elected.

Then, in 2020, during Trump’s fourth year as President—and when he was running for re-election—the global Covid Pandemic hit. Employment went down rapidly. Everyone went home, some working from home, others just not working at all. Businesses closed. Airlines and other sectors slowed down drastically. In March 2020, stock markets around the world crashed. By the end of the first quarter, the U.S. and the world were in a recession because of the Pandemic.
Countries around the world announced stimulus programs to increase government spending and lessen the possibility of a world-wide recession—or even worse, a depression.
The U.S. Pandemic Stimulus in 2020 Changes Everything
The Democrats and the Republicans in Congress, along with President Trump, all wanted to create a federal economic stimulus to help people get through the downturn in business and employment—and prevent a deep recession. The stimulus was also intended to put the economy in a strong position to come back when the Pandemic was over—because everyone believed it would be over before the end of the year, and they wanted to be ready for a strong comeback. Plus, it was an election year and Trump knew a stimulus package would help his re-election. He promoted a big stimulus.
The stimulus was massive. The first major bill was a $2.2 trillion stimulus package passed in March. Along with other stimulus bills, including those that were instituted in the following months, the total amount reached about $5 trillion that went out to individuals and businesses. Both parties in Congress, as well as President Trump, supported it—otherwise it would not have happened. The country had gone into a recession because of the Pandemic, although it was in the final stages of a recovery from the Great Recession. But because of the stimulus, the Pandemic recession was not extreme.
A $5 Trillion Stimulus
It’s hard to compute how effective the stimulus was and in what areas, but it was a $5 trillion input from the Federal Government—a very big chunk of money. There has never been a stimulus that big. It was unprecedented, as was the way it was put into the economy. In order for the stimulus to have an immediate effect, most of the money was sent out directly to the people as checks (many were direct deposits to individual bank accounts), extended unemployment benefits and direct payments to businesses—including small businesses as well as large corporations.
People did not spend it all at once, and many bought items online to be delivered to homes through Amazon and other outlets. These businesses benefited from the Pandemic. Plus, a large part of the stimulus went to major corporations in certain sectors, like the airlines. In fact, all indicators show the rich got richer during this time—along with their tax reduction in 2017. The stimulus was also intended to help individuals as well as businesses—both large and small—to have money to restart the economy after the Pandemic ended.
By the end of the second quarter of 2020, the Pandemic recession was basically over. It was the shortest recession in American history for two reasons. First, because of the stimulus, And second, because the economy had basically recovered from the Great Recession before the Pandemic. That recovery just went on “pause” when the Pandemic hit. But the U.S. economy did not immediately jump into an economic boom. It was gradual. Spending that massive $5 trillion was not immediate, and it took a while before it spread through the recovering economy. Plus, people were cautious. Many just saved their money. It took months before spending went up substantially as the money entered the economy. But you can’t just restart the largest economy in the world overnight.
Although inflation was at a healthy rate around 2% before the Pandemic, by the end of 2020, it had dropped down to a 1.2 % average for the year—basically because of the Pandemic “recession” and the slow recovery in the second half of the year.
Interest Rates and the Pandemic Recession Stimulus
Biden was elected President in November 2020. With the Pandemic basically over, and much of the stimulus money still in people’s pockets, spending slowly increased. Inflation started to creep up with spending, and just two months after Biden took office in January 2021, inflation increased and reached 4.2% in April. * It continued to rise, reaching its biggest increase in 2022. Most economists wondered if this would happen because the stimulus was massive, and there was nothing anyone could do to stop the $5 trillion from being used up. But it was uncharted territory as no Pandemic had ever hit the country as heavily as the Covid Pandemic did.
When the Pandemic suddenly hit in early 2020, the bottom dropped out of the economy. Demand dropped like a rock falling off a high cliff into a deep canyon below. Inflation hit a low of 0.1% in May of 2020—barely above deflation. Powell had lowered the interest rate in February, then again in March and again in April—down to .05%. This continued the trend of lowering the interest rate that Trump wanted in 2019. But it was also lowered because of the Pandemic and economists were delving in unknown territory. This set the stage to help cause the high inflation that would start in April 2021.
Starting in April 2021, when inflation jumped to 4.2%, the Fed rate was at .05% and was kept low, first reaching .07% and then .08% where it stayed until the end of the year. Powell started to raise it in early 2022. By the end of 2021, inflation had continued to rise as people returned to work and started spending as the $5 trillion in stimulus continued to enter the economy that was in full swing. It was like throwing gasoline on the fire of inflation—a disaster waiting to happen. The spending increased through 2022 and beyond—and inflation, although brought under control by raising the Fed interest rate, continued at a lower rate in the following years. †
What is the Best Policy on Interest Rates During a Pandemic?
The Pandemic recession was somewhat unprecedented and how to respond to it was in question. Do you lower interest rates for a Pandemic recession? That would be standard in a “normal” recession. But the Federal Reserve, along with economists, were uncertain if that was the correct policy during a Pandemic recession. Why? Because they knew the Pandemic would end in the coming months and the economy was already strong, having recovered from the Great Recession over the previous 12 years. But still—it was uncharted territory, and all bets were off on what to do and what would happen next.
In looking back, many economists agree that it was a mistake to lower them, since everyone knew the Pandemic and the effects of its recession would be over by the end of the year. But it was an election year and Trump was afraid the recession would go deeper, and he would lose the election. Consequently, he pressured Powell to lower the rates.
Unfortunately, the lower rates helped fuel the upcoming inflation—regardless of who was the next President. Inflation was at an extremely low 0.1% in May 2020. When the Pandemic finally ends, plus the $5 trillion stimulus, and considering the strength of the economy before the Pandemic, inflation was going to skyrocket when it was over. It was actually predictable. But then again—no one had a lot of experience with Pandemics in the modern era and many economists were unsure. In fact, they had no experience.
Next, after months of distributing the stimulus money, came the effects of the massive $5 trillion stimulus, which kept the country from falling even deeper into a recession. But everyone knew the Pandemic would end—and by the end of 2020, it was basically over, and the effects of the $5 trillion stimulus began as spending increased. Businesses re-opened—or came out of their slump—people went back to work, and everyone started spending money like it was going out of style.
Biden Becomes President
Two months after Biden became President in January 2021, demand went straight up quickly from a deep valley of low demand—all causing an incredible rise in prices of everything. Inflation went from 0.1% in May 2020 to 4.2% in April 2021, and then to 5% in May. That was a substantial increase over only two months.
There was nothing that Trump nor Biden could have done to cause it—or to stop it. It was a massive freight train coming down the tracks that was unstoppable. The economy was not only recovering from the Great Recession when inflation was near zero, but from a year of an economic slump caused by the 2020 Pandemic, which put the recovery in “pause” mode.
2021 was followed by a steep rise in inflation in 2022. Donald Trump consistently blamed President Biden for the rise of inflation that started shortly after Biden became President in 2021. Trump constantly blamed him for four years—all the way through the 2024 election (and after). Trump continued to claim that there was no inflation when he was President, and it all started because of Biden’s policies. Trump’s followers believed him, and still do, and that belief was a major factor in Trump’s win in the 2024 election—if not the major factor.
The big question is: Is Trump correct? Did Biden really cause the steep rise in inflation only two months after he took office? If so, then what policies did he enact that caused it?
Or did Trump’s policies during the previous year, and earlier, cause the inflation? And if so, then what policies did he enact that caused it?
What Really Caused the Inflation When Biden was President?
Here are the main causes of the steep inflation which started in April 2021. It’s important to keep in mind that inflation is good if it is generally around 2% a year. At 2% a year, it will rise about 30% every 14 years. In reality, since inflation happens every year, it will hurt the most if your income doesn’t go up with inflation, meaning that the cost of living is what’s important. Income from the lower and middle classes was stagnant, and unemployment was high, from the Great Recession in 2008 through 2022. The wealthy got wealthier during that period. That is the essence of the problem.
In chronological Order:
- The Great Recession in 2008. There is no doubt that if the 2008 recession had never occurred, it is most likely that the high inflation in 2022 would not have happened—even with the Pandemic of 2020. But then again, without that recession, the Presidential and Congressional elections over 14 years might have had different outcomes. But the real pain during the 14-year interval was the cost of living to the middle and lower classes, and if the economy had not fallen into a deep recession, wages would have risen to some extent, although wages for the lower and middle classes have not increased substantially since the 1980s. One cannot say exactly what would have happened, but the Great Recession definitely had a major affect that contributed to high inflation.
- Lowering taxes in 2017. The economic effects of the 2008 Great Recession were slowly healing and on a good course when Trump took office in 2017. His economic policies were centered around lowering taxes for the rich, which caused the national debt to rise substantially. Compared to the wealthy, middle and lower-income Americans received a pittance in tax reduction. And who cares about a tax reduction when you are unemployed? Did the tax reduction input enough money into the economy three years after it was enacted so that it increased demand enough to cause inflation? Not on its own, but any input of money into the economy increases spending—and consequently, inflation.
- Lowering the interest rate in 2019. Trump did not support increasing interest rates when he should have in his first three years. Even though interest rates were increased in 2015 through 2017 because the economy was deeply into the recovery from the Great Depression, Trump opposed raising the rates when Fed Chairperson Powell indicated in 2018 that they should be raised. He urged Powell to lower them, which he did. All economic indicators pointed to raising them, but Trump was concern about his re-election, so Powell lowered them. Even leaving them where they were would have been a better choice. Not raising the rates definitely contributed to the inflation that was still to come. The lowered rates meant that mortgage rates would be low, but with low employment and then the Pandemic, few houses were being built between 2008 through 2020. This drove housing prices up because the population increased and housing didn’t. ††
- The Pandemic and the stimulus in 2020. The Pandemic stimulus was the largest cause of the rise in inflation in 2021-2022. And it was supported by President Trump, the Democrats in Congress, and the Republicans in Congress. Without the support of all three, it would never have passed. $5 Trillion is a large amount of money and there was no stopping its effects once the money was put out there. It was a freight train crash waiting to happen—a perfect storm of inflation.
In Conclusion: Who and What Caused the Inflation?
Trump blamed Biden for the inflation, but Trump played a key role in it, and if one person is to take most of the blame, it is undoubtedly Trump—because he was President for four years right up to two months before the rising inflation began. He did have help, though, because both the Republicans and the Democrats in Congress were the ones who got the stimulus passed. And Biden supported that stimulus before the 2020 election, but he had no official role in it. Then-President Trump strongly supported it because he was thinking about his re-election.
Of course, if there had never been the Great Recession which caused the biggest economic crash since the Great Depression, the massive inflation could have still happened, but as outlined above, the inflation from 2008 to 2022 averaged out to be low over those 14 years. If there had been no steep recession in 2008, it is more than likely that wages/income for the middle and lower classes would have risen, and the cost of living would not have gone up. But then again, the cost of living for the middle and lower classes has not kept up with inflation for the previous 40 years.
And, of course, the Pandemic and particularly the resulting stimulus, caused the inflation to hit all at once, which was the real problem. It should have been spread out over several years and distributed in a different fashion throughout the economy.
But then again, the country had never experienced a Pandemic in modern times, and no one was sure how to manage it.
No one act caused the steep inflation in 2022, but a combination of many factors. It was a “Perfect Storm” of many causes.
All in all, from the Great Recession through 2022, one thing is for certain: The rich got richer and the middle and lower classes got poorer. And that continues today.
“The top 1% owned a record 32.3% of the nation’s wealth as of the end of 2021, data show. The share of wealth held by the bottom 90% of Americans, likewise, has declined slightly since before the pandemic, from 30.5% to 30.2%.” ‡
The Real Problem with the Inflation in 2022 was Low Wages
No one would be complaining if wages had risen in 2008-2022 to meet the cost of inflation. As outlined above, over that 14-year period, average prices rose at a normal healthy rate, but wages were stagnant along with many years of low employment. The average inflation rate was normal over the 14 years. But when inflation got so low that there were periods of deflation, it was like prices dropped into a deep canyon for many years and then when the economy returned—not only from 12 years of recovering from the Great Recession, but also from one year of recovering from the Pandemic—prices climbed out of that deep canyon all at once in a little over one year.
The real pain is always felt by the middle- and lower-income classes and wages have not kept up with inflation for many decades—going back to the 1980s. The problem since the Great Recession in 2008 through 2022 was that it all came to a head in one year—2022.
The rich didn’t mind. They got wealthier when most of the country was suffering losses through higher prices with no rise in wages. The top 10% control 70 percent of America’s wealth and that situation is getting worse.
But there was one other problem: If the rich got richer during that time, where did the money come from? Simple, the national debt went from $10 trillion in 2008 to $33 trillion in 2023. The money came from the federal government and it went into the pockets of the top 10%. Five trillion dollars in pandemic debt alone was enough to explain why the rich got richer during not only the Great Recession, but also during the Pandemic and the high inflation that followed it.
NOTES
* The monthly inflation rate is often misunderstood by many in the general public. If inflation rises 5% one month and then 6% the next month, that doesn’t mean that prices went up 5% the first month and then they rose 6% higher the next month. It means that in the first month, prices were 5% higher than the same month of the previous year, and the following month the prices were 6% higher than the same month the previous year. Over 12 months, the average is taken and that is the annual rate of inflation, meaning how much higher prices were compared to the previous year. For example, if inflation went up 5% every month in a year, then the average inflation that year was 5% that year compared to the same average inflation the previous year.
† Fed Chairperson Powell later admitted to making a mistake by lowering rates in 2019, stating that the economy was in better shape than expected. The Pandemic recession was short-lived, and the higher rates would have helped keep inflation in check—inflation that was still to come.
† † Housing. The biggest increase in the cost of living resulting from the Great Recession combined with the Pandemic was with the cost of housing. The Great Recession was caused by inflated housing prices before 2008 when there were cheap and easily obtained mortgages. This led to overbuilding because inflated home appraisals were given out like candy. After 2008, housing starts almost stopped completely. Housing prices dropped for years afterwards, since there was an over supply caused by easy mortgages before 2008. Housing is often an indicator of economies coming back from economic slumps. Plus, they are an early, but subtle, indicator of economies heading for a crash. Housing starts rarely move quickly because land development, design and construction is a slow process. This is especially true if a subdivision needs to be developed, as they take an extremely long time. Housing started to pick up in 2017 (the most housing starts since 2007) and continued to slowly increase until the Pandemic hit, when starts again almost came to a complete halt. Housing continued to increase, but raising the interest rates caused it to slow down because of mortgage costs. Housing prices remained high through 2024 but are slowly leveling off in late 2024 as mortgage rates creep down.